Clinician Scientist Spotlight : Jesse Fann, MD, PhD

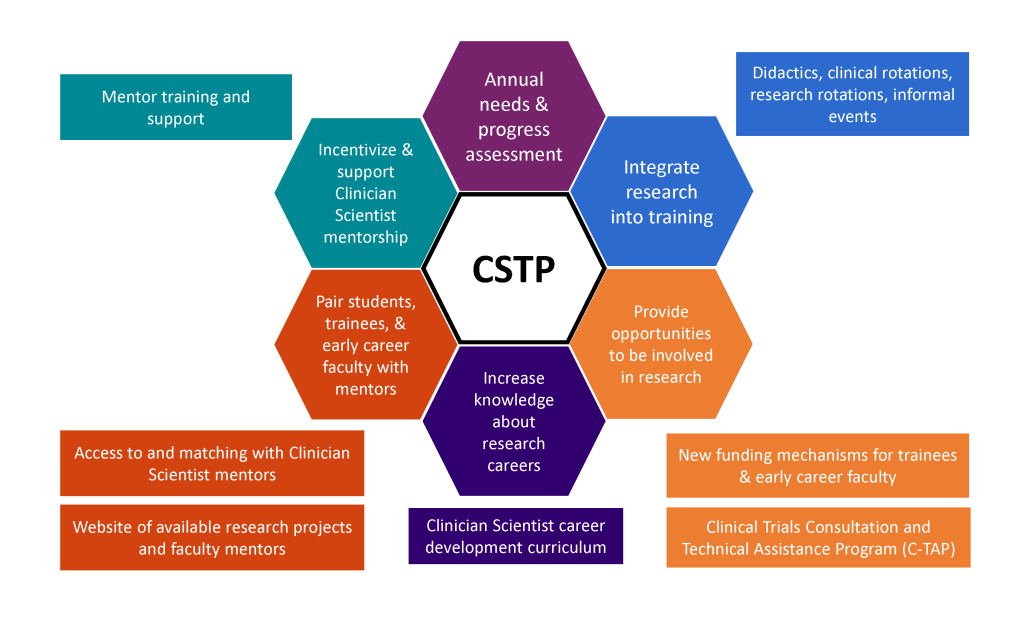
Jesse Fann’s path to becoming a clinician scientist has taken several twists and turns. He was an electrical engineering major in college but, after discovering a fascination with neuroscience and medicine, decided to attend medical school, where he became interested in brain and behavior and decided to specialize in psychiatry. In residency at UW, he developed an interest in neuropsychiatry and C-L psychiatry, so decided to embark on a research project during his R4 year under the mentorship of the late Dr. Wayne Katon. Only then did he realize his passion for clinical research, which led to a T32 research fellowship with Dr. Katon and a faculty position in the psychiatry department in 1995. Over the years, Jesse’s ongoing and diverse clinical roles (inpatient, partial hospital, ECT, C-L, outpatient) have informed many research ideas and funded projects. His current role as Director of the Clinician Scientist Training Program brings together his 30 years of clinical, research, teaching, and administrative leadership experience toward helping to develop and support the next generation of clinician scientists.
Clinician Scientist Spotlight: Rebecca Hendrickson, MD, PhD
 I have a dream job: I work 25% in the PTSD outpatient clinic and on our DBT team, and 75% running clinical trials focused on the biology and treatment of trauma and PTSD. I love that my clinical work directly and continuously informs my research and visa versa. For example, chronic non-specific somatic symptoms like nausea and chronic pain are present at high rates in PTSD, but we know little about why and whether our treatments address them. Similarly, fear of reactive aggression and anger is a common concern for Veterans with PTSD, but doesn’t necessarily respond as robustly to our usual treatments. To address these, our research work now includes detailed assessments of how changes in cardiovascular autonomic regulation relate to symptom burden in PTSD, and how changes in dopamine and noradrenaline regulation after trauma relate to anger and reactive aggression.
I have a dream job: I work 25% in the PTSD outpatient clinic and on our DBT team, and 75% running clinical trials focused on the biology and treatment of trauma and PTSD. I love that my clinical work directly and continuously informs my research and visa versa. For example, chronic non-specific somatic symptoms like nausea and chronic pain are present at high rates in PTSD, but we know little about why and whether our treatments address them. Similarly, fear of reactive aggression and anger is a common concern for Veterans with PTSD, but doesn’t necessarily respond as robustly to our usual treatments. To address these, our research work now includes detailed assessments of how changes in cardiovascular autonomic regulation relate to symptom burden in PTSD, and how changes in dopamine and noradrenaline regulation after trauma relate to anger and reactive aggression.
I took a longer route to get here than was probably required. After an MD/PhD program at Washington University in St. Louis I joined the UW residency program. I participated in the research track, but also completed extensive therapy training, and I cut to part time when I had my second kid. After residency I completed a research fellowship in the VA MIRECC. This allowed me to train in clinical research, which is very different from my PhD work (basic neuroscience). Learning to run interventional clinical trials is an increasingly rare but valued skill set; I feel fortunate to be able to include this in my career, and enjoy providing opportunities for residents to participate as well. I work with residents both as a primary research mentor, and, for residents interested in learning a bit more about analyzing and publishing clinical trials data, on analyses of existing data from our recent trials.
Clinician Scientist Spotlight: Nathan Sackett, MD, MS
 My path to becoming a clinician scientist began when I was a resident physician completing my adult psychiatry training. I saw patient after patient presenting to psychiatric emergency rooms, inpatient units, medical ER’s, and outpatient clinics struggling with the complexities of addiction. As my understanding of addiction increased, so did my frustrated with our treatments. I increasingly felt that therapy or medications were rarely powerful enough to evoke the change needed at a rate that was useful. Around this time, I began to hear stories of folks using a range of psychedelics in a therapeutic setting and seeing amazing results. So, I did what every good trainee does- I scoured the literature and devoured everything I could find about psychedelics. When I read some of the recent studies, I felt I had to pursue it further.
My path to becoming a clinician scientist began when I was a resident physician completing my adult psychiatry training. I saw patient after patient presenting to psychiatric emergency rooms, inpatient units, medical ER’s, and outpatient clinics struggling with the complexities of addiction. As my understanding of addiction increased, so did my frustrated with our treatments. I increasingly felt that therapy or medications were rarely powerful enough to evoke the change needed at a rate that was useful. Around this time, I began to hear stories of folks using a range of psychedelics in a therapeutic setting and seeing amazing results. So, I did what every good trainee does- I scoured the literature and devoured everything I could find about psychedelics. When I read some of the recent studies, I felt I had to pursue it further.
I tried to find anyone in my department or the university doing working in this area, for which there was none. I started the Psychedelic Interest Group and joined the behavioral pharmacology lab of my mentor, Dr. John Neumaier. Now fast forward a few years – I completed my adult psychiatry residency, finished my work in Dr. Neumeiers Lab, completed my addiction psychiatry fellowship and I joined the faculty at the University of Washington. I joined the faculty at UW with the explicit goal of studying how we may use psychedelics to treat addiction, resulting in today’s meeting and the creation of the Center for Novel Therapeutics in Addiction Psychiatry (NTAP).
NTAP started the first state funded psilocybin clinical trial and we’re about to see our first research participants in-person. It’s been a steep learning curve to learn the complexities of doing psychedelic research, but I believe the work will pay off. I also run the Psychedelic Harm Reduction Clinic and can be directly involved in the care of patients who seek to use these substances. It is extremely rewarding to apply the research I am doing directly to the care of my patients, and have my patients inform my research.

 I have a dream job: I work 25% in the PTSD outpatient clinic and on our DBT team, and 75% running clinical trials focused on the biology and treatment of trauma and PTSD. I love that my clinical work directly and continuously informs my research and visa versa. For example, chronic non-specific somatic symptoms like nausea and chronic pain are present at high rates in PTSD, but we know little about why and whether our treatments address them. Similarly, fear of reactive aggression and anger is a common concern for Veterans with PTSD, but doesn’t necessarily respond as robustly to our usual treatments. To address these, our research work now includes detailed assessments of how changes in cardiovascular autonomic regulation relate to symptom burden in PTSD, and how changes in dopamine and noradrenaline regulation after trauma relate to anger and reactive aggression.
I have a dream job: I work 25% in the PTSD outpatient clinic and on our DBT team, and 75% running clinical trials focused on the biology and treatment of trauma and PTSD. I love that my clinical work directly and continuously informs my research and visa versa. For example, chronic non-specific somatic symptoms like nausea and chronic pain are present at high rates in PTSD, but we know little about why and whether our treatments address them. Similarly, fear of reactive aggression and anger is a common concern for Veterans with PTSD, but doesn’t necessarily respond as robustly to our usual treatments. To address these, our research work now includes detailed assessments of how changes in cardiovascular autonomic regulation relate to symptom burden in PTSD, and how changes in dopamine and noradrenaline regulation after trauma relate to anger and reactive aggression. My path to becoming a clinician scientist began when I was a resident physician completing my adult psychiatry training. I saw patient after patient presenting to psychiatric emergency rooms, inpatient units, medical ER’s, and outpatient clinics struggling with the complexities of addiction. As my understanding of addiction increased, so did my frustrated with our treatments. I increasingly felt that therapy or medications were rarely powerful enough to evoke the change needed at a rate that was useful. Around this time, I began to hear stories of folks using a range of psychedelics in a therapeutic setting and seeing amazing results. So, I did what every good trainee does- I scoured the literature and devoured everything I could find about psychedelics. When I read some of the recent studies, I felt I had to pursue it further.
My path to becoming a clinician scientist began when I was a resident physician completing my adult psychiatry training. I saw patient after patient presenting to psychiatric emergency rooms, inpatient units, medical ER’s, and outpatient clinics struggling with the complexities of addiction. As my understanding of addiction increased, so did my frustrated with our treatments. I increasingly felt that therapy or medications were rarely powerful enough to evoke the change needed at a rate that was useful. Around this time, I began to hear stories of folks using a range of psychedelics in a therapeutic setting and seeing amazing results. So, I did what every good trainee does- I scoured the literature and devoured everything I could find about psychedelics. When I read some of the recent studies, I felt I had to pursue it further.