
Scholarly Expertise: Evidence-based practice


Lupita Santillan
Lupita Santillan, PhD, is an Acting Assistant Professor in the department of Psychiatry and Behavioral Sciences. Dr. Santillan is an attending psychologist for the Early Childhood Clinic and the CALMA Clinic at Seattle Children’s Hospital. She is passionate about increasing access to evidence-based early childhood interventions and the provision of mental and behavioral health in Spanish. Her clinical training has focused on providing care to families and children with developmental delays and neurodevelopmental disabilities. Dr. Santillan’s research focuses on the development, implementation, and efficacy of evidence-based behavioral treatments to support children with developmental delays and neurodevelopmental disabilities.

Devon Sandel-Fernandez
Dr. Sandel-Fernandez’s research is focused on predicting impulsive and risk behaviors as they occur in people’s daily lives. She has conducted numerous studies using ecological momentary assessment (EMA) and self-monitoring data from therapy to build person-specific models of symptom dynamics including self-harm, substance use, and suicide attempts.
Dr. Sandel-Fernandez often takes an idiographic (person-specific) analysis approach to answer the question of when in time a person is most at risk for engaging in behaviors they would like to avoid, based on their context, emotions, and personal triggers. Her career goal is to improve treatment outcomes by tailoring evidence-based care to people’s diverse symptom experiences.
Dr. Sandel-Fernandez also studies the use of digital tools and AI in mental health research, training, and treatment. This currently includes: prediction of suicide risk from internet (Google, YouTube, and TikTok) use, a pilot of mobile suicide risk monitoring in UW primary care, and development of an AI-supported simulation training laboratory with simulated patients that trainees can use to hone their clinical skills.

Brenna Emery

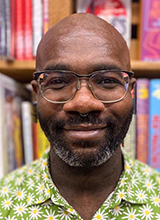
Randall Espinoza
I am currently the Medical Director at the Garvey Institute Center for Neuromodulation and am providing leadership to help grow our portfolio in the area of Neuromodulation and Interventional Psychiatry. Before coming to the UW, I was the Muriel Harris Chair of Geriatric Psychiatry and Professor of Clinical Psychiatry at UCLA. While at UCLA, I held many administrative, clinical and teaching leadership positions including serving as Medical Director of Inpatient Geriatric Psychiatry, Chief of Staff of the UCLA Neuropsychiatric Hospital, Founding Faculty of the UCLA Neuromodulation Division, Medical Director of the ECT and Interventional Psychiatry Program, among others.
I recently became Editor-in-Chief of the Journal of ECT and Related Therapies, the official publication of the International Society of ECT and Neurostimulation. My research projects have included investigating various neuromodulation and interventional therapies and developing novel educational programs and curricula. I have an abiding interest in mentoring and helping faculty at the start of their careers and a commitment to fostering the advancement of women and underrepresented minority (URM) faculty in academic medicine.

Karís Casagrande
Karís Casagrande (she/they), PhD, is a clinical psychologist and director of community outreach at Seattle Children’s Autism Center. She completed her postdoctoral fellowship at University of Washington and Seattle Children’s Hospital, and is an alum of the Leadership Education in Neurodevelopmental and Related Disabilities (LEND) program. Clinically, she specializes in neurodevelopmental assessment, parent coaching models of intervention focused on behavior and social communication, and cognitive-behavioral therapy for individuals with neurodevelopmental differences. She is engaged in community outreach and capacity-building research and programming to improve access to and quality of care for individuals with autism and their families in their home communities. Previously, she was the president of a community non-profit advocacy group and worked with community organizations such as museums, theaters, and hotels to increase accessibility and inclusion for individuals with sensory and developmental differences. She is excited to continue engaging communities and improving accessibility in this new role at the Autism Center.

Sheena Friesen
Sheena Friesen, PhD (she/her), is the attending psychologist for the Child Program on the inpatient Psychiatry and Behavioral Medicine Unit at Seattle Children’s Hospital and Assistant Professor in the Department of Psychiatry and Behavioral Sciences at the University of Washington. She has clinical expertise in disruptive behavior disorders, comprehensive assessment, Dialectical Behavior Therapy, Exposure Therapies, Parent Training, and Trauma-Focused Cognitive Behavioral Therapy.
Dr. Friesen’s research interests broadly focus on advancing knowledge of least restrictive interventions in acute and complex care contexts, trauma-informed care, and interventions designed to address children’s disruptive behavior problems. She has collaborated on and co-led efforts to design and implement a multi-tiered, Modified Positive Behavioral Interventions and Supports (M-PBIS) model of care aimed at increasing positive behavior interventions, reducing restraint and PRN use, and ameliorating racial gaps in care delivery.
Dr. Friesen received her Ph.D. in School Psychology from the University of Washington in Seattle, WA. She completed her pre-doctoral internship training at Johns Hopkins School of Medicine and Kennedy Krieger Institute and went on to complete her postdoctoral fellowship in acute care and clinical psychology at Seattle Children’s Hospital.

Miriam Rubenson

Tessa Frohe
I am a trained Behavioral Scientist with a PhD in Health & Human Performance. The main goal of my work is to reduce substance-related harms and improve quality of life for people experiencing problems related to their substance use. I work closely with community members who use drugs to inform my line of research and address key needs identified. My primary appointment is at the Harm Reduction Research and Treatment (HaRRT) Center within the UW School of Medicine and hold an Affiliate Faculty appointment within the School of Public Health. My aim is to adapt, refine, and disseminate harm reduction programs through digital health interventions to empower individuals and ameliorate substance-related harms.
Jonathan W. Reeves
I am an Acting Assistant Professor and licensed clinical psychologist in the Department of Psychiatry & Behavioral Sciences at the University of Washington School of Medicine. I received my Ph.D. in clinical psychology from the University of California, Berkeley and completed by postdoctoral training at the University of Washington. I am also a consultant for multiple teaching and implementation projects aimed helping community mental health providers deliver effective evidence-based trauma-informed care.
My career goal is to help survivors of complex trauma learn to thrive. My research and clinical work explores how mobile technology, principles of evidence-based practice, and our sociocultural context can be used to help survivors of trauma and their communities recover faster. My work specifically emphasizes recovery from complex racial trauma and other forms of identity-based trauma.
